The Role of Medical Technology in Quality of Life - Urologic Disorders & Pelvic Health
Urologic disorders such as male stress urinary incontinence (SUI), enlarged prostate (BPH) and erectile dysfunction significantly affect the quality of life for men, limiting intimacy and self-esteem. Together, these disorders affect more than 50 million men in the U.S. alone and can be a result of prostate cancer treatments; conditions such as diabetes and heart disease; and pelvic trauma or surgery, among others.
Medical technology interventions and treatments for urologic disorders – including penile implants, artificial urinary sphincters, urethral lifts, male slings and laser therapy – provide alternatives to drugs and may offer more permanent, long-term solutions, ultimately leading to enhanced quality of life.
92% of people with erectile dysfunction reported sexual activity with the penile implant to be excellent or satisfactory.1
For patients with mild to severe SUI treated with a sling published long-term success rates are 62 to 77 percent.2,3
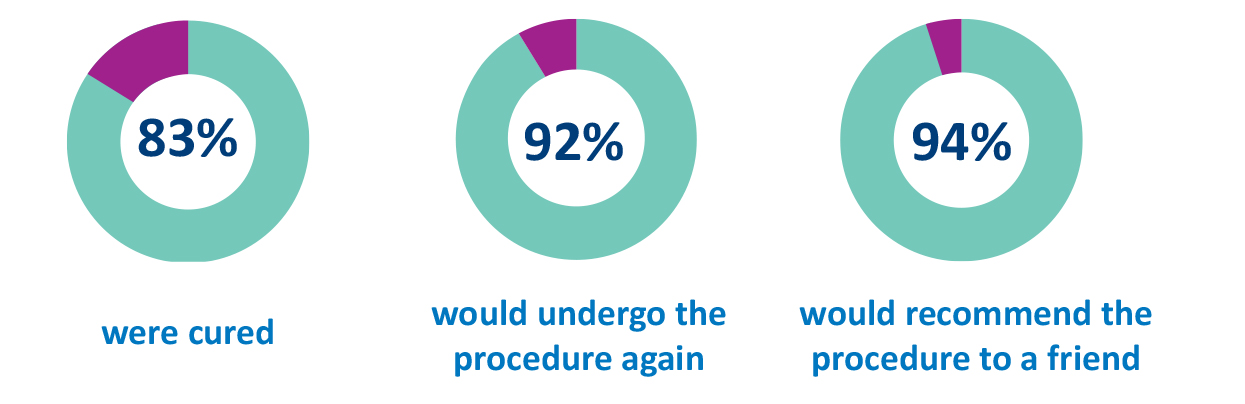
In one study of patients treated with a sling:4
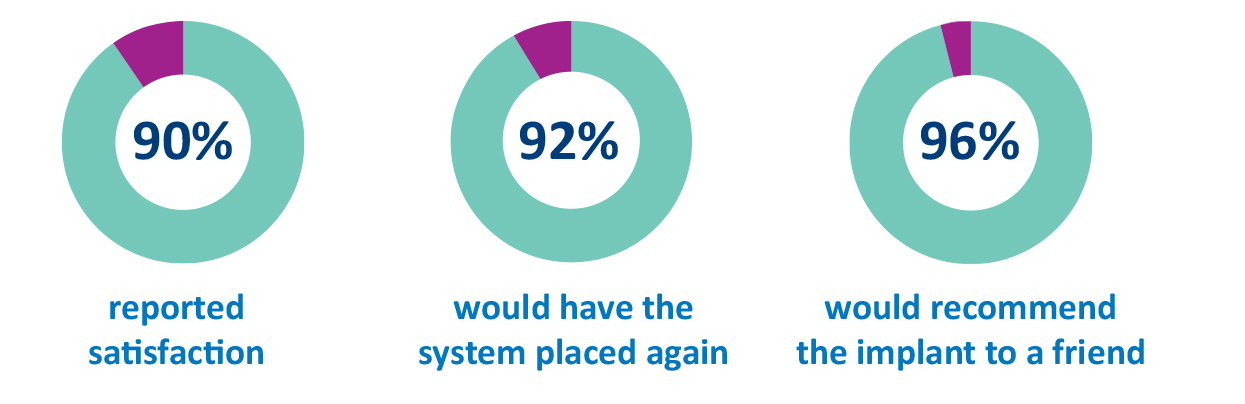
In another study of patients treated with an artificial urinary sphincter:5
For patients with BPH, treatment with laser surgery vs. traditional surgical options is associated with significantly less chance of severe blood loss6; same-day surgery in most cases7; and significantly faster recovery in typical cases.8
[1] Montorsi R, Rigatti P, Carmingnani G, et al. AMS three-piece inflatable implants for erectile dysfunction: a long-term multi-institution study in 200 consecutive patients. Eur Urol. 2000; (37):50-55.
[2] Zuckerman JM, Edwards B, Henderson K, Beydoun HA, McCammon KA. Extended outcomes in the treatment of male stress urinary incontinence with a transobturator sling. Urology. 2014 Apr;83(4):939-45. doi: 10.1016/j.urology.2013.10.065. Epub 2014 Feb 5. PubMed PMID: 24507897.
[3] Rehder P, Haab F, Cornu JN, Gozzi C, Bauer RM. Treatment of postprostatectomy male urinary incontinence with the transobturator retroluminal repositioning sling suspension: 3-year follow-up. Eur Urol. 2012 Jul;62(1):140-5. doi: 10.1016/j.eururo.2012.02.038. Epub 2012 Feb 25. PubMed PMID: 22386196.
[4] The AdVance Transobturator Male Sling: Surgical Tips That Predict Successful Return of Continence Brian Christine*, Mountain Brook, AL, Anthony J. Bella, Ottawa, Canada
[5] Montague, DK. Artificial urinary sphincter: long-term results and patient satisfaction. Adv Urol. 2012:835290. doi:10.1155/2012/835290.
[6] Bachmann A, Tubaro A, Barber N, et al. 180-W XPS GreenLight laser vaporization versus transurethral resection of the prostate for the treatment of benignprostatic obstruction: 6-month safety and efficacy results of the European multi-centre randomized trial – The GOLIATH Study. Eur Urol. November 12, 2013.E pub ahead of press.
[7] Garnick MB. 2013 Annual Report on Prostate Diseases. Boston, MA: Harvard Health Publications; 2013.
[8] Bachmann A, Tubaro A, Barber N, et al. 180-W XPS GreenLight laser vaporization versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6-month safety and efficacy results of the European multi-centre randomized trial – The GOLIATH Study. Eur Urol. November 12, 2013. E pub ahead of press.